Description of Meniscal Root Tears
Both the medial and lateral menisci have a stout attachment at their very posterior aspects, which are called the root attachments. These root attachments are important because they hold the meniscus in place, provides stability to the circumferential hoop fibers of the meniscus, and prevents meniscal extrusion.
When there is a tear of the meniscal root, it has been demonstrated on biomechanical testing that it is equivalent to having the whole meniscus removed. Thus, a tear of the meniscal root is considered a very serious condition.
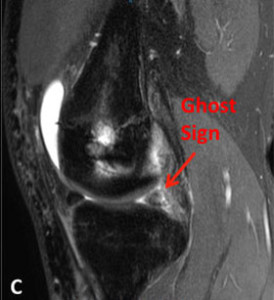
Here is a perfect example of the early sequelae of a medial meniscus root tear:
There are two different group of patients who suffer meniscal root tears:
- The first group consists of athletes in their 20s who sustain the tear with trauma. This could include an injury to the ACL, PCL, and other associated ligament combinations. In these circumstances, the meniscal root is commonly torn along with the ligament, and it is recommended to perform a concurrent meniscal root repair. Failure to repair the meniscal root tear in these circumstances can lead to the development of osteoarthritis, failure of a cruciate ligament reconstruction graft, and other problems further down the line.
- The second group of patients who commonly tear their meniscal root is adults in their 50s. The consequences of a meniscal root tear appear to be much more severe in this age group. A meniscal root tear, which can occur with minor or seemingly trivial trauma, with a pop in the back of their knee with deep flexion, squatting and lifting, and other activities, can be quite severe. It is in this group of patients for which the rapid development of osteoarthritis can occur. In some of these patients, rather significant bone swelling, insufficiency fractures, and the appearance of osteonecrosis (avascular necrosis), can obscure one to seeing that it was caused by meniscal root tear.
Have you sustained a meniscal root tear?
There are two ways to initiate a consultation with Dr. LaPrade:
You can provide current X-rays and/or MRIs for a clinical case review with Dr. LaPrade.
You can schedule an office consultation with Dr. LaPrade.
(Please keep reading below for more information on this condition.)
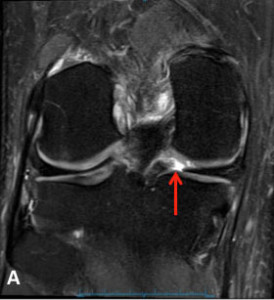
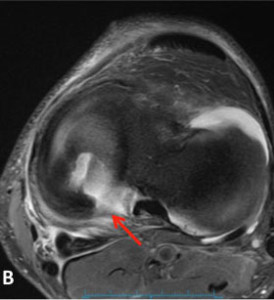
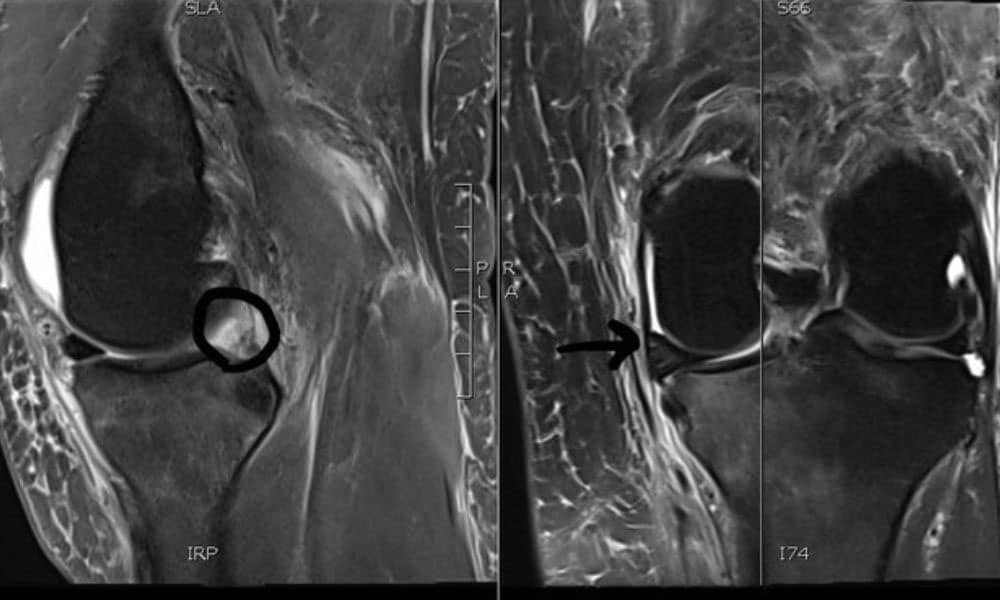
MRI Diagnostic
Meniscal Root Tear Meniscal root tears can be seen on coronal, axial and sagittal MRI views. On the sagittal view, as seen in Figure C, there is a “ghost sign” which is indicative of meniscal root tear. A normal, healthy meniscus should look like a dark black triangle; however, as this figure shows the meniscus is much lighter or “ghosted” representing the root tear.
How to Read a MRI of a Meniscal Root Tear
Treatment for Meniscal Root Tears
The treatment of meniscal root tears in older patients can be very difficult. This is because they are not commonly diagnosed until the progression of arthritis is more severe. Due to the increasing knowledge that these tears can lead to rather progressive arthritis, one should consider an attempt at a meniscal root repair at the first signs of the development of pain and swelling with activities, which usually indicates the progression of arthritis, joint space narrowing, or any bony edema of the affected compartment on MRI scans. A concurrent distal femoral or proximal tibial osteotomy may also be indicated if the patient is malaligned to unload the affected compartment.
Meniscal root tears have only been noted as a significant pathology over the last 5 to 6 years. Research into the problem is ongoing. Our lab has noted that radial tears adjacent to the root attachment, known as a radial root tear, can also cause the same problems as a meniscal root avulsion of the attachment site. Our studies have also demonstrated that repairs of these radial root tears can restore fairly normal weightbearing characteristics and load sharing of the affected compartment. Thus, in properly selected patients, a radial root repair would also be indicated.
Post-Op
Patients who have a meniscal root repair need to be non-weightbearing for 6 weeks after surgery. Physical therapy is initiated on the first day after surgery. Patients are limited in moving their knees to 90 degrees of knee flexion for the first two weeks after surgery and then after this time they may increase their knee motion. At six weeks after surgery, a partial protective weight bearing program is initiated and patients may slowly wean off crutches when they can ambulate without a limp. The use of a stationary bike may be also started. Patients should avoid impact activities, deep squats, squatting and lifting, and sitting cross-legged for a minimum of 4 months after surgery to protect the meniscus root repair.
Related Studies
- Anatomic Analysis of the Posterior Root Attachments of the Menisci
- Posterior Root Avulsion Fracture of the Medial Meniscus
- Not Your Father’s (or Mother’s) Meniscus Surgery
- Anterior Intermeniscal Ligament of the Knee – An Anatomical Study
- Popliteomeniscal Fascial Tears Causing Symptomatic Lateral Compartment Knee Pain
- Prospective Outcomes Study of Meniscal Allograft Transplantation
Meniscus Root Tear FAQ
1. What is a meniscus root?
The meniscus root is where the main body of the meniscus attaches to the bone. There are meniscal root attachments both in the front and back of the tibia.
2. What is a meniscus root tear?
A meniscus root tear happens when the root attachment is torn or destabilized. Most meniscus root tears actually are not the root tearing, but actually a tear of the meniscus within 1 cm of the root. These are called radial root tears and are about 90% of all meniscal root tears. A meniscus root tear can totally destabilize the shock absorbing function of the meniscus and can lead to insufficiency fractures, spontaneous osteonecrosis of the knee (SONK) and early onset arthritis in patients.
3. Meniscus root tear versus sprain?
Meniscus root tears can be either complete or partial. Our classification has called a partial root tear as a type 1 tear, and these can usually be trimmed without any significant consequence to the knee. Complete radial tears, which are type 2 tears, always should be considered for repair in patients who may need them, to prevent the development of osteoarthritis.
4. Meniscus root tear versus IT band syndrome?
Iliotibial (IT) band syndrome usually occurs on the outside of the knee over the bony bump called the lateral epicondyle. It is usually an overuse problem due to repetitive running in patients who have a tight iliotibial band. As such, iliotibial band friction syndrome usually does not occur until an athlete has been running for around 2 miles when the pain will start on the outside of the knee.
A medial or lateral meniscus root tear usually has pain within the center of the knee. These tears hurt with deep squatting or flexion activities and often lead to joint line pain. These symptoms are usually totally different between iliotibial band syndrome and meniscus root tears.
5. Meniscus root tear versus patellofemoral symptoms
It is not uncommon for patients who are in their 50s or 60s with meniscus root tears to also have concurrent patellofemoral chondromalacia (a kind term for arthritis). Thus it is important to differentiate the location of the pain in the knee to determine if it is coming from a potential meniscus root tear or from the patellofemoral arthritis. Usually, patients with pain in their kneecap joint have pain with squatting and lunges right on the front of their knee, whereas patients with meniscal root tears usually have pain in the very back of the knee, especially with deep squatting activities. In addition, patients can have the meniscus slip out of the joint, called extrusion. This can also sometimes be quite painful and can help to differentiate between patients who may have some preexisting patellofemoral arthritis (kneecap arthritis) and those that may have a meniscus root tear.