Femoral Condyles – Anatomy:
The femoral condyles are located on the end of the thigh bone, or the femur. They are covered by articular cartilage and function as a shock absorber for the knee.
Femoral Condyle Chondromalacia:
Damage to the cartilage on the end of the bone is known as arthritis. This could also be described as “chondromalacia” which is basically a “kind” term for arthritis. Any damage to the cartilage in the body in effect is arthritis.
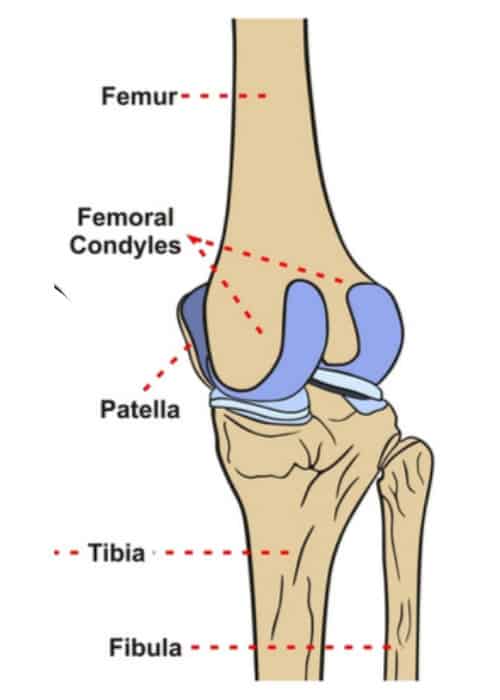
Femoral Condyle Location:
There are two femoral condyles. The medial femoral condyle is located on the inside part of the knee whereas the lateral femoral condyle, which is bigger, is located on the outside part of the knee. The femoral condyles articulate, or contact, with the tibia and on the medial side this is in the medial tibial plateau and the medial meniscus and on the outside of the knee is known as the lateral tibial plateau in the lateral meniscus.
Femoral Condyle Treatment:
Cartilage damage can be treated in many different ways. First, if there are rather large amounts of arthritis with cartilage thinning, a program of physical therapy to work on strengthening of the muscles so one has better absorption and puts less stress across the knee, can be indicated. Injections of biologic agents (bone marrow aspirate concentrate (BMAC), or platelet rich plasma (PRP)), corticosteroids, or viscosupplementation injections may also be utilized to try to decrease some of the irritation of the joint lining which can cause pain from arthritis.
Chondroplasty:
When the cartilage defect is more localized, surgery may be indicated. Surgery can consist initially of cleaning up the rough edges and seeing how the patient does. This is called a chondroplasty. It is important to recognize that with a chondroplasty one does not cure a cartilage problem and is mainly dealing with a mechanical irritation due to the rough cartilage edges. This may be indicated in smaller lesions in patients who may not be candidates for more advanced cartilage treatment to help deal with the mechanical symptoms.
Femoral Condyle Cartilage Defect:
For other femoral condyle cartilage defects, it is important that one follow the basic principles of cartilage replacement to ensure the maximum outcome. This includes having an opposing cartilage surface be normal (the medial or lateral tibial plateau), having the shock absorber on that same side be intact or nearly intact (the medial or lateral meniscus), having the weight bearing of the joint not pass into that compartment (not being bowlegged (varus) or knocked knee (valgus)), and ensuring that the ligaments of the knee are intact. Most commonly, this is ensuring that the ACL is intact. If one fits all of these criteria, or one can be treated with surgery to correct these criteria, then one could be a candidate for a cartilage resurfacing procedure. If one has a problem with the ligament instability or is maligned, or the meniscus is not intact, the chances of a cartilage surgery working are significantly diminished.
Femoral Condyle Cartilage Replacement Surgery:
Cartilage replacement surgeries commonly depend upon the size of the defect and the quality of the remaining cartilage edge. This is called the cartilage margin “shoulder”. A smaller defect with good cartilage shoulders can potentially be treated with a microfracture. In this procedure, small holes are made in the bone to try to induce some localized bone marrow elements, which may include stem cells, to form a fibrocartilage healing response. Microfracture procedures are best indicated for small and well localized defects, commonly those that are 1 cm or less in size and have normal bone surfaces below the defect. Another type of treatment can involve taking a plug of bone and cartilage, called an osteochondral transfer, from area of the knee and transferring it to the other area of the knee.
Osteochondral transfer -vs- Osteoarticular Allograft:
This type of transfer is also best in small defects It may be used when a microfracture may not be indicated, such as in patients who have bone cysts below a small area of a cartilage defect. In this case, replacing both of the bone and cartilage would be indicated. Larger cartilage defects are best treated by more advanced surgeries, which often involve replacing all of the cartilage surface or the bony cartilage surface. The current gold standard is a fresh osteoarticular allograft. In this procedure, the bone and cartilage units are replaced by somebody who has recently died (an allograft), and replacing the whole bone and cartilage unit. This type of surgery is considered the “gold standard” because the cartilage has an excellent chance of healing and if one follows a proper rehabilitation program with low impact activities only for the first year after implantation, there are excellent outcomes described in the literature for this procedure. It is important to recognize that one has to be matched to a donor, which means somebody has to die for one to obtain a fresh osteoarticular allograft, and that the basic principles of placement are carefully followed, such as ensuring that the depth of the bone for the fresh allograft are as little as possible, and certainly no more than 1 cm of total bone, or there is a higher risk that the bone will not heal in and ultimately the graft will fail. Other potential cartilage replacement procedures include growing one’s cartilage and re-implantation, called a autogenous cartilage implantation procedure, and using other types of allograft or autograft cartilage pieces for implantation. These surgeries certainly may be indicated in some areas, but the gold standard is still the fresh osteoarticular allograft if possible.
Femoral Condyle Cartilage Defect Treatment:
Treatment of cartilage defects of the femoral condyles requires a thorough workup and ensuring that the defects are truly symptomatic. An incidental finding on MRI scan may not need treatment, and close observation may be indicated in these cases. It is important that we treat the patient and not treat the MRI scan because some patients may have a cartilage defect and because they have normal strength and motion of their knee they may not have symptoms and may not have progression of the defect for a long time, if at all. Therefore, it is important to asses that these cartilage defects are causing symptoms to the patient before embarking on much bigger surgeries because the consequences of having a failed cartilage procedure are often worse than the symptoms that one has prior to having the cartilage surgery performed on a minimally or non-symptomatic knee.
For more information on femoral condyle conditions and the available treatment options for your knee pain, please contact the offices of Dr. Robert LaPrade, serving patients from the Twin Cities, Minneapolis-St. Paul, Edina and Eagan, MN.
