What is the Meniscus?
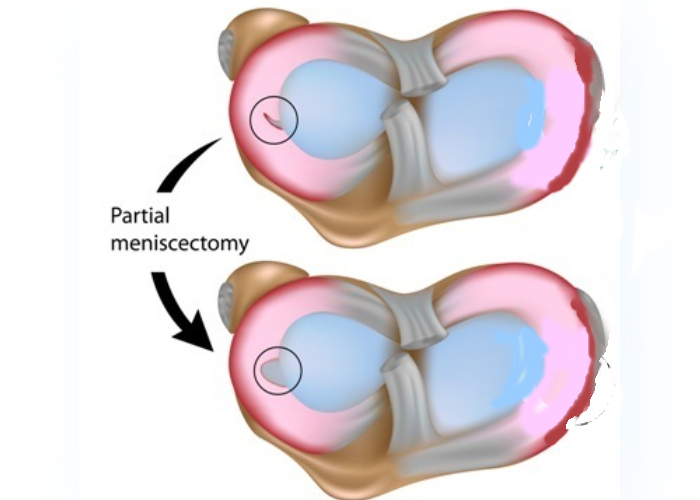
The menisci are essential shock absorbers for the joint. They are also important for normal gait and stability of the knee. We are just starting to understand the role that a partial meniscectomy has on a patient’s overall gait pattern, their subsequent muscle weakness, and the overload of the joint that occurs when a partial meniscectomy needs to be performed. Unfortunately, the majority of the time a meniscus tear is not able to be repaired because of its poor blood supply and the fact that the inner part of the meniscus in the joint is so thin that it often cannot be sutured. However, because of its vital role in all these factors, it is important to try to repair a meniscus tear if at all possible to try to preserve joint health.
Effects of a Partial Medial Meniscectomy
Arthroscopic partial medial meniscectomy is the most common outpatient surgery in the United States. However, meniscus injury and subsequent resection contributes to a 7 times greater risk for developing knee osteoarthritis later in life. While it is generally believed that most patients have an uncomplicated recovery following an arthroscopic partial medial meniscectomy, a close look at patients demonstrates that at least 1 out of 3 continue to have quadriceps strength deficits, subsequent overloading of the knee joint due to poor absorption from this muscle weakness, and decreased physical function which can last for months to years. Thus, quadriceps weakness can be one of the most modifiable risk factors to slow down the progression of arthritis after an arthroscopic partial medial meniscectomy. A physical therapy regimen that is started immediately after surgery can better prevent and address persistent strength deficits and activity limitations following an arthroscopic partial medial meniscectomy. It is important to decrease postoperative pain, work on immediate restoration of quadriceps voluntary activation, and restore joint motion. Through this, the potential to improve overall lower extremity and quadriceps strength and physical function would help to minimize the risk of knee arthritis progression. It is important to recognize that quadriceps weakness increases overall knee joint loading, and arthritic changes can initiate as early as 2 to 5 years after an arthroscopic partial meniscectomy. Thus, there is a critical early window to try to work on addressing muscle inhibition and restoring strength to the joint to slow down the progression of arthritis after a meniscectomy.
Are you suffering from the effects of a partial meniscectomy on your articular cartilage?
There are two ways to initiate a consultation with Dr. LaPrade:
You can provide current X-rays and/or MRIs for a clinical case review with Dr. LaPrade.
You can schedule an office consultation with Dr. LaPrade.
(Please keep reading below for more information on this condition.)
Partial Meniscectomy on Articular Cartilage
Young athletes who have undergone a partial or full meniscectomy due to a meniscus injury or prior non-treated ACL tears have a very high chance of developing osteoarthritis later in life, which has been found to be between 65% to 90% of the time. Overall, osteoarthritis is a degenerative articular cartilage joint disease that is characterized by articular cartilage maturation and hypertrophy, cartilage matrix degeneration and erosion, and osteophyte (bone spur) formation, and because of this it is a leading cause of disability in the United States, affecting a third of the population 65 years or older. The unfortunate thing is that there are no existing disease modifying osteoarthritis drugs that can effectively prevent, slow down, or treat osteoarthritis. In addition, there are no specific surgical interventions to reliably repair partial articular cartilage lesions to prevent the progression to end-stage arthritis. The current way that the majority of cases of osteoarthritis in older patients are managed is by treating the symptoms of pain and inflammation with exercise, corticosteroid injections, viscosupplementation and ultimately total joint replacements.
Untreated meniscal tears, including macerated tissue tearing, has been reported to be a known risk factor for the development of arthritis over a 2-1/2 year time, with an almost 5 times increased risk of arthritis. In addition, a total meniscectomy increases the risk of arthritis by 14 times at 21 years postoperation and a partial meniscectomy increases the risk of arthritis by 4 times 16 years after surgery.
Effects of Meniscectomy on Gait Mechanics
It is also known that patients who have a meniscectomy have gait mechanics that are altered because of the lack of meniscal support. Patients who have undergone partial medial meniscectomies have been reported to have increases in external rotation in walking which can overload the cartilage. These small increases in rotation may result in the thinner cartilage, which is not adapted to receiving as much force, being the main source of joint loading over time and could lead to the further progression of arthritis in these patients. In addition to these structural changes after a meniscectomy, knee motion also is consistently decreased in operative versus contralateral limbs. Thus, early physical therapy to restore motion is an important portion of the patient’s postoperative rehabilitation. In addition, it is important to recognize that the small alterations and joint kinematics can over time have large effects on the cartilage and lead to arthritis.
It is assumed that in addition to loss of mechanical function and shock absorption from the meniscus tear, inflammation develops in the joint after an injury. The inflammatory response often will set off cytokines, specifically interleukin-1 and tumor necrosis factor alpha (TNF –alpha), which can lead to the development of cartilage wear and breakdown. In addition to meniscal damage after traumatic injury, it is known that obesity or aging (or both), can also result in increased inflammatory cytokines in the knee joint over time. Thus, a means to slow down this increased systemic inflammation should be indicated.
In addition to the local effects on the cartilage of inflammatory cytokines causing cartilage wear, it is also important to recognize that the acute inflammation can lead to increased pain. Pain can also result in modification of the patient’s gait, which can change the load pattern and lead to further cartilage wear. In addition, it is well recognized that a patient with a varus knee alignment will have greater medial cartilage overload and the same is true for the valgus aligned knee having more lateral cartilage overload after a meniscus resection in the same (ipsilateral) compartment. Thus, losing the meniscus and the affected compartment when one has a joint malalignment will cause the cartilage to wear out even faster over time. It is important to recognize it is not just a surgical meniscectomy that can cause these changes. Meniscal damage without a meniscectomy can still lead to significant changes in the location and amount of load the articular cartilage which can lead to arthritis. Thus, it is important to judge if a patient has pain, which can lead to changes in gait mechanics and muscle strength, as an important indication to proceed with a meniscectomy to slow down the progression of arthritis, even if it is a degenerative tear.
