What is Spontaneous Osteonecrosis?
Spontaneous osteonecrosis of the knee used to be felt to be due to an idiopathic cause, which meant we just did not know what caused it. It was generally found in middle-age women and often there would be rapid development of osteoarthritis of the medial femoral condyle, often with an insufficiency fracture. In the past, many of these patients went on to need total knee replacements within months to a few years.
What Causes Spontaneous Osteonecrosis?
We now know that almost all cases of spontaneous osteonecrosis of the knee are due to previously unrecognized medial meniscal root tears. In these circumstances, often with a squatting-type position, such as when cleaning floors, doing gardening, or with deep flexion with sporting activities such as skiing, the meniscus root would tear off its attachment in the back of the knee. In many patients, the meniscus root tear would then proceed to slip out of the joint, which we call extruding, and that basically removes the main cushion to prevent arthritis on the inside part of the knee. It has been found biomechanically that when one does have a meniscus root tear, that it is equivalent to having all your medial meniscus taken out.
How to Treat Spontaneous Osteonecrosis
The treatment in patients who have fairly normal cartilage surfaces still remaining and who have spontaneous osteonecrosis of the knee is to repair the meniscus root tear if possible. In these circumstances, restoring the cushion to the knee, getting the meniscus root tear to heal, and the period of nonweightbearing on crutches which is required for the root tear to heal, almost always results in the healing of the spontaneous osteonecrosis of the knee, even when there was an insufficiency fracture.
Thus, it is currently felt that most cases of spontaneous osteonecrosis of the knee that are caught early enough can be treated. No longer do patients need to require a partial or total knee arthroplasty because the diagnosis is in doubt. Most cases are due to a posterior horn medial meniscus root tear with extrusion and early diagnosis and treatment is recommended to slow down the progression of arthritis in these patients.
Spontaneous Osteonecrosis of the Knee Injury FAQ
Spontaneous osteonecrosis of the knee, often referred to as SONK, was historically referred to as an insufficiency reaction of the medial femoral condyle that occurred “spontaneously” could often go on to have insufficiency fractures and advanced arthritis of the medial compartment of the knee. It was typically described in middle-aged women and the etiology was not well known. What is now known is that most cases of spontaneous osteonecrosis of the knee are due to meniscus root tears that were not well recognized as a pathology in the past.
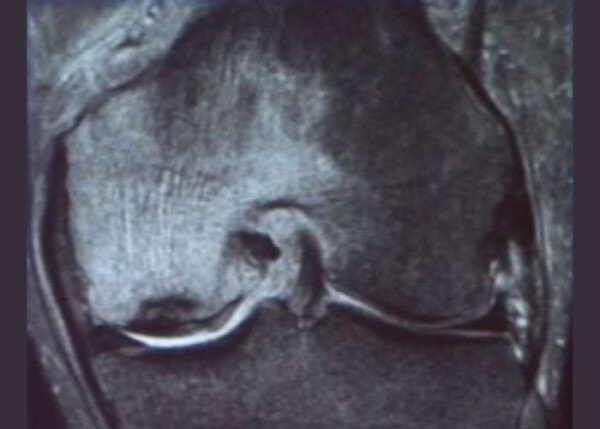
Meniscal root tear with SONK and an insufficiency fracture in a left knee
1. What is spontaneous osteonecrosis of the knee?
Spontaneous osteonecrosis of the knee is due to an overload of the medial compartment, primarily the medial femoral condyle, leading to a swelling of the bone on MRI and an overload of the articular cartilage surface. This overload can lead to insufficiency fractures and the rapid wear of the articular cartilage. As our profession has become better educated about meniscus root tears, we now recognize that almost all cases of spontaneous osteonecrosis of the knee are due to posterior horn type 2 medial meniscus root tears.
2. What does spontaneous osteonecrosis of the knee look like on MRI?
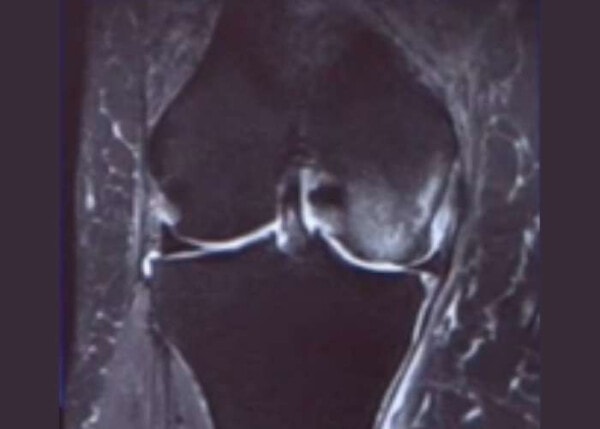
Spontaneous osteonecrosis of the knee on MRI often shows diffuse increased signal on the fat suppression images of the medial femoral condyle. Insufficiency fractures close to the subchondral bone and articular cartilage surface are not uncommon. Concurrent with this, a meniscus root or radial root tear of the posterior horn of the medial meniscus is often present.
3. What symptoms are present with spontaneous osteonecrosis of the knee?
Most patients who develop spontaneous osteonecrosis of the knee would have initially felt pain in the back of their knee and often a pop while they were gardening, laying carpet, washing floors or doing activities with deep knee flexion. Then, a few weeks later, they would start to develop rather significant pain on the inside of their knee, which can be due to overload of the medial femoral condyle bone and articular cartilage due to the meniscus root being nonfunctional. When there is a meniscus root tear, it can often extrude outside the joint, which makes the cartilage surfaces articulate directly against each other. In some people, this can result in the rather rapid development of arthritis.
4. What is the treatment for spontaneous osteonecrosis of the knee (SONK)?
The treatment for SONK is to first determine its cause. If it is a meniscus root tear and the articular cartilage is still pretty much intact, even if there is an insufficiency fracture, performing a meniscus root repair and then allowing the knee to quiet down during the 6 weeks when the patient would be nonweightbearing often results in resolution of the SONK. For patients who have rather significant arthritis already, the use of crutches and possibly a medial compartment unloader brace may allow the bone to heal and then have an assessment after that as to the need for a partial or total knee arthroplasty.

Coronal MRI image of a right knee with a medial meniscus root tear and “SONK” of the medal femoral condyle due to overload of the medial compartment caused by the extruded medial meniscus
5. Why does spontaneous osteonecrosis of the knee develop sometimes after arthroscopic surgery?
Spontaneous osteonecrosis of the knee is felt to be due to an overload of the articular cartilage and bone on the medial compartment of the knee. If there is a trimming of the meniscus root or a radial tear which effectively makes the meniscus nonfunctional, this overload due to the lack of cushion effect of the meniscus could lead to spontaneous osteonecrosis of the knee. This is felt to be the major cause of SONK after knee arthroscopic surgery.
6. Is a bone scan useful for spontaneous osteonecrosis of the knee (SONK)?
While a bone scan can show bone turnover and show increased activity on the medial femoral condyle with SONK, an MRI scan is a more definitive and useful study because it can show the underlying cause of SONK, which more than 80+% of the time is due to a meniscus root tear or a radial root tear.
7. Is there an association between spontaneous osteonecrosis of the knee and osteoporosis?
Most cases of meniscus root tears occur in middle age women. Often, these middle age women may have some underlying osteopenia or osteoporosis. In addition, if they have been disabled for a period of time due to their medial compartment knee pain, the bone may appear to be relatively osteopenic. Thus, while some of these patients may have osteoporosis, it is important to recognize that most cases of SONK are due to meniscus tears rather than having underlying osteoporosis.
8. What is the association between medial meniscal extrusion and spontaneous osteonecrosis of the knee?
Most cases of meniscus extrusion are due to a type 2 medial meniscus root tear. Other types of meniscus extrusion can include a complete radial tear where the meniscus becomes nonfunctional or patients who may have diffuse arthritis and the meniscus extrudes outside the joint. The most common cause of SONK is a meniscus root tear, and meniscus root tears often have extrusion of the meniscus outside the joint, which can lead to the overload causing SONK. Thus, most cases of SONK would be expected to have some form of meniscus extrusion present.
