Description of Trochlear Dysplasia
One area of the knee that is not discussed as often as some of the other components, is a section called the trochlea. This area of the knee is easy to identify. When the knee is bent, the undersurface of the kneecap (the patella) lies in an area known as the trochlear groove. The sides of the patella and the walls of the groove should be almost parallel. The normal shape of the trochlea groove is concave. In fact, the outside, or lateral aspect of the trochlea groove has a higher bump than the inside part. This allows the patella, or kneecap, to glide down the central aspect of the distal femur rather effortlessly due to its bony constraints. This is important because the patella serves as a fulcrum to increase the overall strength and efficiency of the quadriceps muscles of the thigh.
When the trochlea is flat, or even possibly has a convex or dome shape, it is known as trochlear dysplasia which usually is referred to as an unstable kneecap. In these circumstances, the trochlea is not shaped normally, and the patella does not have the normal bony constraints to provide stability. Thus, one needs to rely on the medial patellofemoral ligament and their quadriceps mechanism to hold the patella in place.
Symptoms of trochlear dysplasia:
- Knee pain and knee aching
- Higher risk of patellar dislocations and instability
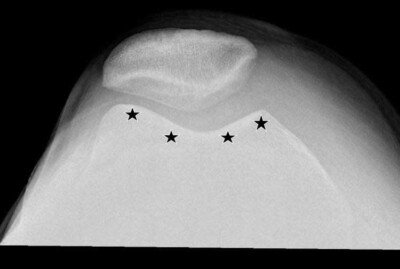
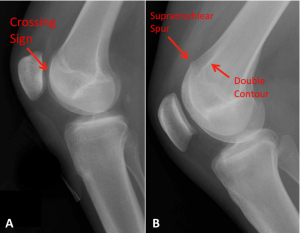
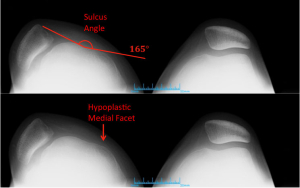
A diagnosis of trochlea dysplasia is usually made by a thorough physical exam and radiographic work-up. Patients with trochlear dysplasia often have increased medial and lateral patellar translation near full extension and at 45 degrees of knee flexion. They may also have an apprehension test where they feel their patella is going to dislocate laterally. On plain X-rays, one can see a “crossing sign” on the lateral knee X-ray that would indicate that the trochlea groove is both flat and shallow. The 45-degree patella X-ray would also show a decrease in size of the groove, flattening, and sometimes a dome shape. A frontal view, or AP, radiograph may show some hypoplasia, or a decrease in size, of the medial femoral condyle.
Are you experiencing trochlear dysplasia symptoms?
There are two ways to initiate a consultation with Dr. LaPrade:
You can provide current X-rays and/or MRIs for a clinical case review with Dr. LaPrade.
You can schedule an office consultation with Dr. LaPrade.
(Please keep reading below for more information on this condition.)
MRI Diagnositc
Crossing Sign for Trochlear Dysplasia
Trochlear dysplasia is often assessed on lateral radiographs. Figure A shows a crossing sign representing a shallow trochlea. A dysplastic trochlea can also include a supratrochlear spur as well as a double contour which represents the hypoplastic medial trochlear facet.
CLICK IMAGE TO ENLARGE
Treatment of Trochlear Dysplasia
The treatment of trochlear dysplasia can be very difficult. It is important to have a thorough workup to include a patient’s overall alignment, their tibial tubercle–trochlea groove angle (TT–TG), and an MRI scan to evaluate the status of the articular cartilage of their patellofemoral joint. This is important because surgical treatments may not always be indicated if there is significant arthritis present. In addition, a plain X-ray to look at the amount of patella alta, or a high-riding patella, is indicated.
The treatment of trochlear dysplasia can be very difficult. Patients who have a lateral patellar dislocation have a much higher risk of recurrence when they have trochlear dysplasia. Because the severity of trochlea dysplasia can run from minor to severe, treatment options are also varied. They can include a reconstruction of the medial patellofemoral ligament, a tibial tubercle osteotomy, a trochleoplasty, where the distal aspect of the femur is cut and reshaped to create more of a normal groove, a distal femoral osteotomy, and other associated treatments. Thus, no one patient has the same treatment as another, and a thorough workup is necessary to determine the best course of action, if any, for a particular patient with trochlear dysplasia.
Post-Op
Patients who have a trochleoplasty need to be non-weightbearing for 6 weeks after surgery. They are also placed into a continuous passive motion (CPM) machine for 6-8 hours a day while they are non-weightbearing. Motion is usually restricted to 90 degrees of knee flexion for the first two weeks after surgery and then increased to full knee motion as tolerated. After x-rays show sufficient healing of the trochleoplasty at 6 weeks postoperatively, patients are allowed to initiate weight bearing as tolerated and may wean off crutches when they can walk without a mill. The use of a stationary bike is also started with low resistance. After 3 months postoperatively, patients may initiate endurance and agility exercises. Full activities are allowed in patients without arthritis in their patellofemoral joint upon passing a sports test, usually at 7-9 months after surgery.
Trochlear Dysplasia FAQ
In most knees, there is a groove on the end of the femur, called the trochlea, in which the kneecap sits. This provides a certain amount of bony stability to the kneecap joint to prevent it from sliding, mainly to the outside. When this groove is flatter or completely flat or concave in shape, the bony stability that is normally present is absent and is a much higher risk of having the patella dislocate or partially dislocate (sublux5-) to the outside.
1. What is trochlear dysplasia?
Trochlear dysplasia is a condition whereby the normal “V” shape of the trochlea is relatively flat or dome shaped. The usual classification for this is a Dejour classification.
2. Is trochlear dysplasia genetic?
Most cases of trochlear dysplasia are believed to be genetic. There may be some cases where somebody sustains a kneecap dislocation that is not put back in place when they are young and developmentally the trochlear groove may not form normally, but overall most cases of trochlear dysplasia are felt to be genetic.
3. Is trochlear dysplasia rare?
Severe cases of trochlear dysplasia are rare, whereas more mild cases where the trochlear groove may be flatter than normal, are not that uncommon. Therefore, it is a relatively common condition, but often does not cause significant problems when it is a milder case of trochlear dysplasia.
4. How often does patella alta occur with trochlear dysplasia?
It is very common for patella alta to be present with trochlear dysplasia. This is because a patella can sit up high above the trochlear groove and it is possible that developmentally a trochlear groove may not form as deep of a groove if the patella is not sitting within it as well as in some patients compared to those whose patellar tendon height is normal.
5. What is the role of trochlear dysplasia in patellofemoral instability?
Lateral dislocations of the kneecap are fairly common, especially in adolescents. Those that have a normal trochlear groove geometry have a relatively lower risk, varying between 5% and 15%, of having recurrent dislocations. Those who have some form of trochlear dysplasia have a much higher rate of recurrent dislocations, which can be 30% to 50% depending upon how flat their trochlear groove may be.
6. How is trochlear dysplasia diagnosed on x-rays?
Trochlear dysplasia is best diagnosed on both a 45-degree patella sunrise view and also on the lateral x-rays. On the lateral knee x-rays, the femoral condyles may not overlap normally and there can be what is called a crossing sign, which indicates the trochlea is not fully developed. In addition, a supratrochlear spur can also be present laterally, which can indicate a more severe case of trochlea dysplasia. On the patella sunrise views, one can measure the sulcus angle and determine the relative flatness of the trochlear groove.
7. How is trochlear dysplasia diagnosed on MRI scans?
MRI scans may give a more definitive assessment of the shape of the trochlear groove compared to plain x-rays because they will show the soft tissue cartilage interface. There are times on x-rays where the trochlear groove may appear to have a slight groove, but in reality the trochlear groove is flat or dome shaped when one takes into effect the shape of the articular cartilage. Therefore, correlating the x-ray findings to the MRI findings, especially on the axial cuts on the MRI scan, can be useful to determine the extent of trochlear dysplasia present.
8. What is the role of trochleoplasty with trochlear dysplasia?
For patients who have severe trochlear dysplasia, such as severe type B trochlear dysplasia, the risk of recurrent patellar dislocations can be quite high. For those patients who have had multiple dislocations, the shape of the trochlea should be assessed to determine if a reshapening of the end of the femur, called a trochleoplasty, may be beneficial to help restore their function. Determining who may need a trochleoplasty as a first-stage surgery requires an extensive workup, but for those patients with significant trochlear dysplasia who have had recurrent dislocations after soft tissue reconstructions, the concurrent role of trochleoplasty for the revision surgery becomes more definitive.
9. What types of knee braces may work for trochlear dysplasia?
It may be very difficult for knee braces to prevent the patella from sliding to the outside with significant activities when one has had recurrent lateral patellar dislocations and has severe trochlear dysplasia. Those braces that may have the ability to work would have to have buttresses to pull the patella medially as well as straps to try to provide some static stability to the knee that is lost when the trochlear groove is relatively flat.