Posterior Cruciate Ligament Reconstruction
If you are experiencing pain in the ligament behind the knee, you may be a candidate for PCL knee surgery.
The posterior cruciate ligament, or PCL, is the strongest ligament of the knee. While the anterior cruciate ligament, or ACL is injured more often than the PCL and is more commonly discussed, a torn PCL accounts for more than 20% of reported knee injuries. The ACL sits in front of the PCL location in the knee. A torn PCL is commonly missed and left undiagnosed.
The posterior cruciate ligament’s most important function is to prevent posterior translation of the knee at higher knee flexion angles. Thus, patients commonly complaining of problems with deceleration, problems going down stairs and inclines or general twisting, turning or pivoting activities.
PCL injuries are classified according to the amount of injury to the functional ligament:
- Grade 1 PCL Sprain: partial PCL tear
- Grade 2 PCL Tear: near complete PCL tear
- Grade 3 PCL Tear: a complete PCL tear – the ligament is non-functional
CT scan of a failed ACL reconstruction demonstrating the wide diameter of the previous ACL tibial reconstruction tunnel. In some patients, these tunnels will become larger than when they were originally reamed, especially for hamstring autografts or cadaver allografts. If they are larger than 12 to 14 mm in diameter, or are in a position where an anatomic positioning of the ACL reconstruction graft would break into the previously malpositioned tunnel, then a two-staged surgery would be recommended. This would involve bone grafting of the tunnels and, once the tunnels heal in approximately four to six months, to proceed with a revision ACL reconstruction in the correct anatomic position.
CLICK IMAGE TO ENLARGE
When to Have PCL Surgery
In general, Dr. LaPrade will perform a PCL surgery on all injuries that present themselves as a grade 3. In a higher level athlete, it may be recommended to proceed with a PCL reconstruction sooner because the results of acute reconstructions are much better than chronic reconstructions.
When Dr. LaPrade does find that a patient needs PCL surgery, he thoroughly assesses the patient to see if there is a concurrent injury. In our hands, approximately 90% of patients who have a symptomatic PCL tear limiting their function also have a posterolateral corner, posteromedial injury or other associated injury. Thus, the incidence of isolated PCL reconstructions in our own series is approximately 10% of the total PCL reconstructions performed.
Are you experiencing persistent PCL symptoms? When conservative treatments fail, you may be a candidate for a PCL knee reconstruction.
There are two ways to initiate a consultation with Dr. LaPrade:
You can provide current X-rays and/or MRIs for a clinical case review with Dr. LaPrade.
You can schedule an office consultation with Dr. LaPrade.
(Please keep reading below for more information on this treatment.)
Double-Bundle PCL Reconstruction
Our surgical rehabilitation technique for a surgical PCL reconstruction is a double bundle reconstruction with allografts. We use a double bundle reconstruction because historically, the results of PCL reconstruction in the literature have been less than ideal. Dr. LaPrade participated in an international symposium of PCL specialists in Florence, Italy in November 2002. At this symposium, all the current anatomy, biomechanics, clinical outcomes and diagnostic methods for PCL ligament injuries and PCL tears were closely reviewed. It was felt, at that point, the outcomes for PCL reconstructions were less than ideal and it was recommended that newer reconstruction and rehabilitation techniques be evaluated. In addition, it was felt rehabilitation had a much stronger effect on the results of a PCL reconstruction compared to an ACL reconstruction and a rehabilitation program was established to maximize patient outcomes.
PCL Surgery Video
PCL Reconstruction Success Rate
Dr. LaPrade has found that a double bundle PCL reconstruction has been extremely effective in restoring knee stability back to the patient both objectively with PCL stress x-rays as well as subjectively based on patients independently evaluating their outcome scores.
Dr. LaPrade’s surgical PCL reconstruction technique involves the creation of a closed socket tunnel in the femur for both the anterolateral and posteromedial bundles of the PCL. The graft is fixed in that location and pulled distally down the tibia. The anterolateral bundle is fixed at 90° of knee flexion with an anterior force on the knee and distal traction on the graft. After the anterolateral bundle is fixed to the tibia at 90° of knee flexion, the posteromedial bundle is next fixed in full extension.
PCL Rehab Program
Our PCL rehab program allows patients to initiate prone knee flexion at 0-90° on day one. The patients use a PCL brace, preferably a PCL Rebound brace, for 6 months postoperatively at all times, except to shower or change clothes, to reduce the posterior gravitational stress to the knee. We also recommend that high level athletes utilize a PCL Rebound brace at least through the completion of the first competitive season after the PCL reconstruction to unload the PCL graft and protect it while it remodels.
We have found that our rehabilitation program, which may be considered aggressive by other treatment centers, has not resulted in any of our grafts stretching out over time and has demonstrated a much quicker return of knee motion, decreased risk of knee stiffness and higher level of function.
Related Studies
PCL Reconstruction FAQ
1. How long does it take to recover from a sprained PCL? How long does it take to recover from a PCL tear?
The time that it takes to recover from a PCL tear depends upon how severely the PCL is torn. For a very minor sprain, which would be called a grade 1 PCL tear, athletes may be able to return back to competition within 2 or 3 weeks. This usually requires that the swelling in the knee has resolved, strength is returning, and the athlete’s endurance and agility have returned back to normal. For a grade 2 PCL tear, where there may be more instability of the knee, it may take up to 6 weeks for a sufficient recovery without surgery. In these cases, the use of a dynamic PCL brace, such as the PCL rebound brace, may help to hold the knee in a more reduced position so when the PCL heals it is not loose. For a grade 3 PCL tear, where a significant increase in posterior tibial translation occurs because of the PCL tear, it is becoming more widely accepted with improved PCL reconstruction techniques that these cases undergo surgery. While some of these cases may respond well to a dynamic PCL brace holding their knee into a more reduced position, it is also important to recognize that patient reported outcomes after PCL reconstruction surgeries are much better when performed in the first few weeks after injury rather than waiting for 6 weeks or longer. Thus, when one does have a grade 3 PCL tear and feels instability, surgical reconstruction would be indicated. In these circumstances, it takes from between 9-12 months to completely heal after a PCL reconstruction.
2. Can a PCL injury heal on its own?
Unlike the ACL, the PCL does have an ability to heal. The synovial membrane around the PCL allows for some healing to occur. What is important to recognize is that in these circumstances, the effects of gravity can be bad on a PCL healing. Thus, when one does have a severe PCL tear, one should consider either a cast or a dynamic PCL brace to hold the knee into a reduced position so that the PCL has the best chance of healing in a “tighter” rather than a loose position.
3. What is PCL reconstruction surgery? What is PCL surgery?
PCL reconstruction surgery consists of replacing the torn PCL with one’s own tissues or an allograft. Most of the time in the United States, due to the large size of the PCL, allograft tissue is used to reconstruction the posterior cruciate ligament. The PCL has very wide attachment on the femur, and many surgical techniques today are using a double-bundle PCL reconstruction technique to reproduce that wide attachment site. Clinical studies so far report that knees who have double-bundle PCL reconstructions (which are placed in the correct positions) do better in terms of their overall stability at follow-up than those with single-bundle PCL reconstructions.
4. How successful is PCL surgery?
Until the last 10 years, it was felt that PCL surgery was not very successful. This was because the anatomic and biomechanical studies on the PCL had not been done in detail and PCL reconstructions were not put in an anatomic position. Over the last 5-10 years, anatomic-based PCL reconstructions have been validated biomechanically and to date in clinical studies, double-bundle PCL reconstructions have been found to be equal to the outcomes for ACL reconstructions. Thus, most studies can successfully reconstruct the PCL 85-90% of the time.
5. How long does PCL surgery take?
The length of a PCL surgery depends upon whether there are other injuries present. Almost 90% of the time with a PCL tear, there are other ligaments that are also torn. Thus, this can greatly affect the overall surgical time. In our hands, an isolated double-bundle PCL reconstruction takes from 35-40 minutes to perform. If there is a concurrent posterolateral corner or medial-sided knee injury, this may add another 60 minutes to the procedure. When there are all 4 ligaments in the knee torn, the total time to place all the grafts and fix them can be up to 2 hours.
6. When to have PCL surgery?
Currently, it is recommended that almost all patients and athletes who sustain a grade 3 PCL tear should consider a reconstruction. Patients with grade 2 PCL tears should consider reconstruction if they have trouble decelerating, going down inclines, going down hills, or if they start to develop pain in their kneecap joint or along the inside (medial joint line) of their knee. Medium to long-term PCL tears often lead to patellofemoral and medial compartment arthritis, so pain in these locations should be carefully watched. In general, one should have PCL stress x-rays to determine the grade of a PCL tear. It is felt that PCL stress x-rays which show more than 8 mm of increased posterior tibial translation on the injured knee compared to the contralateral knee should consider surgery. If it is less than 8 mm, it may indicate that the patient is guarding or that there is a partial PCL tear. In these circumstances, a rehabilitation program would be indicated first followed by a repeat x-rays to make sure that the PCL is not completely torn at a later date (usually 2-3 weeks later).
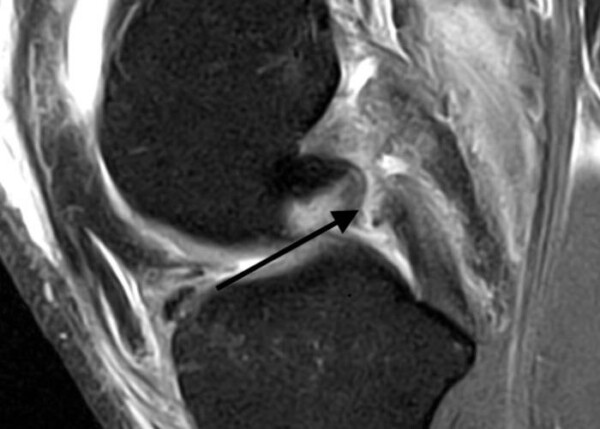
Arrow shows a PCL tear in 16 year old
7. What is a double-bundle PCL reconstruction?
A double-bundle PCL reconstruction takes into account the wide attachment site of the PCL in the femur by using 2 separate grafts to reconstruct this area. There is still only 1 tunnel on the tibia where both grafts pass through. A double-bundle PCL reconstruction has been found to better restore knee biomechanics and has been shown in clinical studies to better restore knee stability than a single-bundle PCL reconstruction. Not all surgeons perform double-bundle PCL reconstructions because it is felt to be technically difficult. However, the technique that we have developed and taught is quite easy and double-bundle reconstruction for the PCL is very similar to a single-bundle PCL reconstruction and only takes about 5 minutes longer.
8. What is double-bundle PCL tensioning?
The 2 bundles of the PCL act together and reciprocally. It is important to recognize that the 2 bundles need to be tensioned at different positions. The main bundle of the PCL is the anterolateral bundle. This bundle should be fixed first and fixed at 90 degrees knee flexion. This best helps to set the tibia at the correct tibiofemoral step-off point. The posteromedial bundle of the PCL is the smaller bundle, and is more important in knee extension. We have found that this bundle should be tightened second, after the anterolateral bundle and should be tightened with the knee out straight (in full extension).
9. What is PCL reconstruction recovery time?
The PCL takes longer to heal in, and thus requires more biologic healing time, than an ACL reconstruction. This is because a PCL is larger and a larger graft is used to reconstruct the PCL. Most PCL rehabilitation programs rely on a 6-week period of nonweightbearing, utilizing a dynamic PCL brace, followed by a program up to 6 months postoperatively whereby a patient/athlete avoids running, twisting, turning and pivoting. At the 6-month point, if the PCL stress x-rays show good healing of the PCL reconstruction, patients can initiate a jogging program and start side-to-side activities if they have sufficient quadriceps strength and do not have any valgus collapse when they perform a single-leg squat. In our hands, with our professional and Olympic athletes, they are generally able to return to full competition between 9 and 12 months postoperatively. This totally depends upon whether there is solely an isolated PCL reconstruction or if there are other concurrent ligaments that are torn for the PCL.
10. What is a PCL reconstruction protocol?
A PCL reconstruction rehabilitation protocol needs to be individualized to the patient’s injury. In general, PCL reconstructions undergo 6 weeks of non-weightbearing and perform motion exercises on their stomach with prone knee flexion. This negates the effects of gravity and helps the PCL to heal without having to worry about stiffness. At the 6-week point, patients initiate weightbearing and they wean off crutches when they can ambulate with a limp. They generally work on straight-ahead (single-plane) activities until the 6-month point. Thus, they are allowed to work on a stationary bike and graduate to the use of an elliptical machine to build up their quadriceps mechanism, but should allow the graft to heal sufficiently prior to doing higher level activities so the PCL graft does not stretch out with time. During the first 6 months postoperatively, patients wear a dynamic PCL brace to ensure that the effects of gravity do not cause the graft to stretch out. We have found that this dramatically improves the results of PCL reconstructions and feel it is essential to obtain the best outcomes.
11. PCL repair versus reconstruction?
PCL repairs are generally indicated for bony avulsions, which almost always occur off the tibia. In these circumstances, an incision can be made over the back of the knee and screws can be placed through the bony avulsion to hold it in place. It is generally not recommended to repair midsubstance PCL tears or PCL tears with a lot of stretch in them because these tears have a higher risk of stretching out, and these patients often get stiff because the suture repair does not allow for early range of motion without the risk of the PCL repair stretching out. Thus, PCL reconstructions are indicated in the vast majority of cases, except where a PCL may have a bony avulsion which can be repaired back. In those patients with a bony avulsion which is repaired, they should be placed into the PCL dynamic brace to ensure that if there is any intrasubstance stretch of the PCL, the brace would hold the knee in the correct position so that the PCL repair would not heal in a lax position and become loose over time.
12. Is a PCL reconstruction necessary?
The PCL is the strongest ligament in the tear. When it is torn completely, patients can have extra motion in the knee and have difficulty going down hills, down stairs, or down inclines. The literature supports the fact that patients who have chronic tears of the PCL in these circumstances usually have arthritis developing within 5 to 7 years. Therefore, for patients who do have significant instability, the current recommendation is to proceed with a PCL reconstruction. It is important to recognize that historically PCL reconstructions did not do as well as ACL reconstructions and often surgeons stop performing PCL reconstructions when they found out their outcomes were no better than what the patient initially started with. However, with modern anatomic-based techniques, especially with a double-bundle PCL reconstruction, the outcomes are much better and have been validated in the literature to have outcomes that are equal to the outcomes of ACL reconstructions.
13. What is an arthroscopic PCL reconstruction?
Most PCL reconstructions are performed with arthroscopy or arthroscopic assistance. They involve the preparation of grafts, most commonly cadaver grafts (allograft) for the PCL grafts, and also reaming tunnels and fixing the grafts in the tunnels. Large studies have validated anatomically and biomechanically that the double-bundle PCL reconstruction best restores stability to the knee, and also appears to stretch out less than a single-bundle reconstruction does over time. Therefore, we recommend a double-bundle PCL reconstruction to address complete tears of the PCL.
14. When is weightbearing started after a PCL reconstruction?
There has not been a lot of scientific studies to document when it is safe to start weightbearing. However, we do know that there is a higher risk of having PCL reconstructions stretch out over time. Therefore, most centers will keep patients nonweightbearing or limited weightbearing with the knee out straight for a period of 6 weeks to maximize early healing of the PCL reconstruction grafts in the tunnels.
15. How does one diagnose a PCL tear on x-rays or MRI?
A PCL tear can be diagnosed both with stress x-rays, plain x-rays which may show an avulsion fracture, and with MRI scans. In general, the results of MRI scans are excellent when the PCL tear is acute, which means it just occurred in the last few weeks. However, the PCL does have a chance to heal, often in a loose position, and it is difficult to interpret this on the MRI scans. MRI scans for chronic PCL tears are not very accurate with an accuracy of probably between 60% and 70%. Therefore, the use of PCL stress x-rays is indicated in most circumstances for both acute and chronic injuries to have an objective number to determine how bad the PCL tear may be. It is our recommendation that all patients who have PCL tears, whether acute or chronic, have PCL stress x-rays so one can be objective about the amount of instability that is present and whether they need surgery or not. Stress x-rays of >8 mm usually will require surgery.
16. Where is the femoral tunnel placed for a PCL reconstruction?
It has been proven that biomechanically having the graft as distal as possible, which means having it up against the edge of the articular cartilage, best restores the function of the PCL. Therefore, the anterolateral bundle of the PCL should be centered between the trochlear point and the medial arch point and brought up against the articular cartilage. The posteromedial bundle of the PCL sits further back from the cartilage and below the anterolateral bundle and this reconstruction tunnel should be positioned after the anterolateral bundle reconstruction tunnel has been placed to best measure where it should be located. In general, we ream the 7-mm tunnel for the posteromedial bundle so that the anterior edge of the tunnel should be 5 to 6 mm back from the edge of the articular cartilage.
17. What are common reasons for PCL reconstruction graft failure?
One of the most common reasons for PCL reconstruction graft failure is having the graft placed in a non-anatomic position. This can cause the graft to stretch out over time. In addition, reaming a PCL reconstruction tunnel and taking out one of the root attachments, can lead to early arthritis and having a PCL reconstruction graft stretch out over time also. .
18. Can a PCL reconstruction be performed using a quadriceps tendon?
In general, the majority of the PCL reconstruction literature has been published using allografts. This is because the PCL is such a large structure that it is difficult to obtain large enough grafts to be able to reproduce its function with autografts. However, in some countries where allografts are not available, the use of autografts is indicated. In these circumstances, using the quadriceps tendon to replace the anterolateral bundle and one of the hamstring tendons to replace the posteromedial bundle has been reported in the peer-reviewed literature to be a successful option for this. However, in general, we try not to have the quadriceps mechanism be shut down with harvesting the quadriceps tendon because the quadriceps mechanism is an essential component for PCL rehabilitation postoperatively.
19. When is a brace necessary for PCL reconstructions?
The current gold standard of care is felt to use a dynamic or static PCL brace to protect the graft such that early motion can be an issue right after surgery. In general, having a brace that can push the tibia forward when the knee bends has been shown in the literature to help with the success rate of PCL reconstructions. These dynamic PCL braces have also been demonstrated to be effective for acute tears because the PCL can often heal when it is just stressed out, and holding the knee in a reduced position often can result in the knee having the chance to heal acutely when it is not completely torn.
20. What can one expect for the first couple of months after a PCL reconstruction?
In our hands, we start physical therapy on day 1 after a PCL reconstruction. The patient is allowed to work on prone knee flexion, whereby they are lying on their stomach, from 0 to 90 degrees. We allow this motion because it takes away the negative effects of gravity when one is on their stomach. They also start using a dynamic PCL brace between days 3 and 5 postoperatively, when their skin incisions will allow this, and the amount of swelling is decreased, such that the knee can be held in a stable position and they can work on knee motion. It is important to recognize that the majority of PCL reconstructions are performed with other ligament reconstructions, so this also needs to be taken into account. After 2 weeks, we allow the patients to increase their prone knee flexion to as much as they can tolerate. At the 6-week point, they are allowed to initiate a partial protected weightbearing program and may slowly wean off of crutches when they can ambulate without a lift. We usually have patients participate in lower impact activities, such as cycling or the use of an elliptical machine, with wearing their PCL dynamic brace, until the 6-month point. PCL stress x-rays are repeated at that point in time. If it shows that the PCL graft is healing well, one can start an impact program and start to wean out of the PCL dynamic brace. A full return to activities is usually allowed when they can pass a functional sports test of some type between 9 and 12 months postoperatively.
21. What is the killer turn for a PCL reconstruction?
The killer turn for a PCL reconstruction is described in the literature as occurring with patellar tendon grafts. The patellar tendon graft is relatively thin and where it crosses the back part of the tibia, there can be an area that can wear on the graft when one has it placed through a tibial tunnel rather than having it secured directly to the tibia, called in in-lay procedure. However, the “killer turn” has not been described with using other soft tissue grafts, and is believed to primarily have been due to the use of patellar tendon allografts or autografts and possibly what is potentiated by the effects of gravity in patients who do not have a dynamic knee brace to hold their knee into a correct position.
22. What is PCL avulsion surgery?
It is not unusual to sometimes see that a PCL tears off the tibia with a piece of bone. Commonly, the meniscal root attachments may also be attached to this piece of bone. In this circumstance, we try to bring these patients to surgery if their knee feels unstable within the first days to weeks after the injury to try to place sutures or screws and washers through the fragment to reduce it. The recovery time when the PCL can be “repaired” in this circumstance is significantly lower than having a complete reconstruction and also restoring the meniscus roots back to their anatomic position is an important way to best restore knee function. Therefore, for patients who do have some instability with a PCL avulsion fracture, performing a surgery to fix the fragment is usually indicated.
23. What is the return to sport time after a PCL reconstruction?
It is important to understand that a PCL reconstruction is a more complicated surgery and that rehabilitation needs to be slowed down to allow the larger grafts to heal in. If one returns back to activities prior to sufficient healing, the PCL reconstruction can stretch out over time. This is especially true for single-bundle PCL reconstructions in patients that have a flatter tibial slope. In general, we want the patients to have good restoration of their balance, agility, and overall endurance, and pass a functional sports test at approximately 9 to 12 months after a PCL reconstruction to be able to return back to full activities.
24. What are the risks of not having a PCL reconstruction with a grade 3 tear?
It has been commonly reported that many athletes can get back to full activities after a PCL tear. Often times, they may have 5 to 7 years of their careers extended by treating it with a nonoperative method. However, having seen the residual of many of these cases, the knee often wears out over time and these patients often end up with a sore and painful knee 5 to 7 years later. Therefore, with the improved techniques that have been developed as well as the outcomes that have now been reported to be equal to that of isolated ACL reconstructions, the current gold standard among PCL reconstruction surgeons is to reconstruct the PCL in these athletes to best prolong their careers and prevent the development of osteoarthritis over time.



